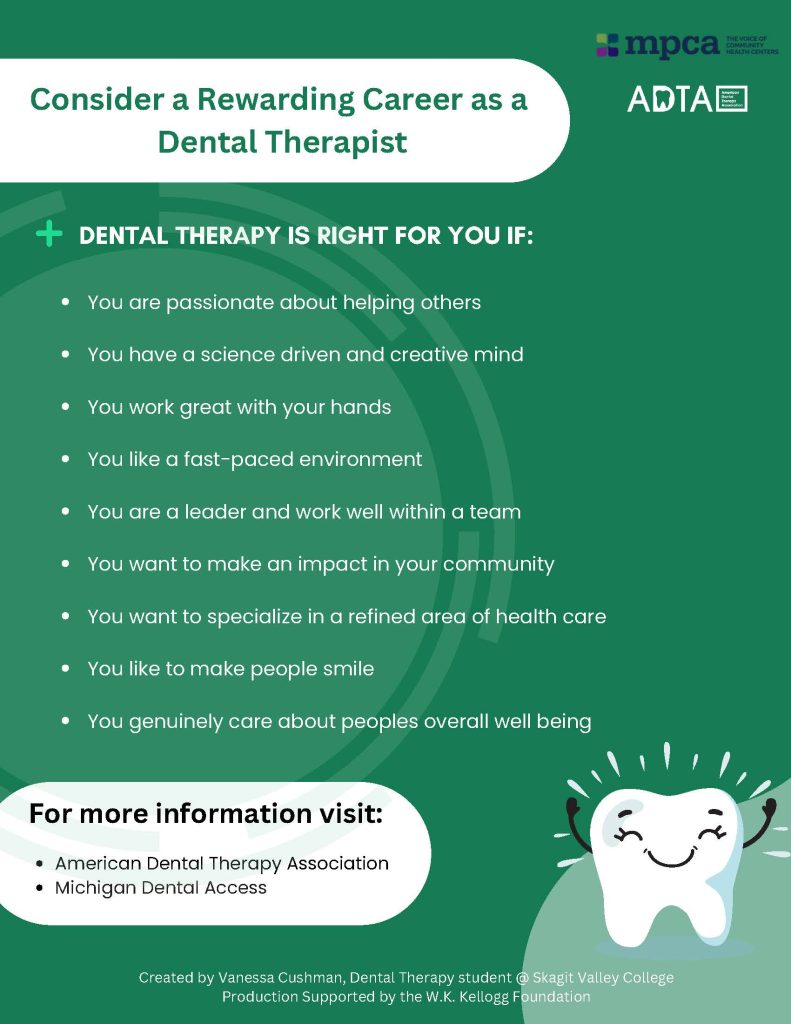
My name is Dana Obey, a Dental Therapy student at Skagit Valley College, where our program director organized a community rotation with the ARCORA Foundation in Longview, Washington. As a Dental Therapist, it’s important to learn a variety of delivery systems accessible to patients, and I’m happy to share my most memorable encounters during the rotation and highlight the importance of teamwork and personalized care in addressing the needs of vulnerable populations. I had the opportunity to work with a diverse patient population, each facing unique barriers to dental care. I’ve learned so much, not only about the technical aspects of dental care but also about the importance of communication, collaboration, and understanding the specific needs of underserved communities. Working with patients who had complex medical histories, socio-economic challenges, and limited access to care reinforced my appreciation for innovative, collaborative approaches to dental treatment.
One of the most impactful experiences during my rotation involved a high-risk geriatric veteran with multiple chronic health conditions, including HIV, high blood pressure, a history of stroke, and prior spinal surgery. These medical challenges made traveling for dental treatment difficult, compounded by long wait times at the local Community Health Center and limited dental services through the Veterans Administration (VA). As a result, the patient had gone without necessary dental treatment for several years.
The Smile Mobile dental bus played a crucial role in providing care. This mobile unit allowed us to deliver services directly to the patient, addressing his immediate dental needs. In collaboration with the supervising dentist, I adjusted his partial dentures, which had recently become damaged when two anchor teeth fell out. This temporary treatment helped restore some of his chewing function and comfort, allowing him to function until he could access permanent dental care and establish a “dental home.” The patient was extremely grateful for the immediate relief, especially since the care was provided at no cost. We also connected him with a denturist who could assist with future adjustments, and the patient expressed relief knowing he would be able to use his dentures for another year before being eligible for a new set through the VA.

This experience highlighted the critical role of mobile dental care in reaching patients who are unable to travel for care, particularly elderly veterans in rural or underserved areas. The Smile Mobile proved to be a vital bridge to care, and integrating dental therapists into these mobile units can further expand logistical and financial access to dental services for high-risk populations.
Another memorable encounter was with a young man, aged 25-30, who had recently entered a Suboxone treatment program after struggling with drug addiction. He sought dental care for extensive caries on his anterior teeth and expressed a strong desire to “fix things” now that he was in recovery. This patient shared that he had not fully realized the extent of the dental damage caused by his past lifestyle until he had something to smile for again. His renewed commitment to his oral health reflected his broader efforts to improve his overall life.
During our consultation, I learned that the patient was eligible for up to $4,000 in dental treatment assistance through his tribe. To access this benefit, he simply needed to establish a dental home and submit his treatment needs to the tribe. This financial support was crucial in making dental care more accessible and affordable for him, especially after overcoming the significant challenges of addiction. The patient’s excitement about the resources available to him underscored the importance of community-based programs that support individuals in need. It was a powerful reminder that local health organizations and tribal resources can play a pivotal role in improving access to care for underserved populations.
This encounter emphasized the importance of understanding local healthcare resources and the role they play in addressing patients’ needs. It also highlighted the significance of patient empowerment—by being aware of and accessing available resources, patients can make informed decisions about their care and take control of their health. In this case, the patient’s ability to receive financial assistance for dental care was a key factor in helping him move forward in his recovery journey, which reinforced my commitment to advocating for access to care through mobile units and increasing the number of dental providers in underserved communities.

I also worked with patients at a local Wellness Center, particularly focusing on a young recovering addict who required full-mouth rehabilitation due to extensive caries and years of neglect. Throughout his treatment, I noticed his remarkable progress, not only in terms of dental health but also in his personal growth. Despite the challenges many patients at this facility face—such as difficulty with compliance and frequent no-shows—this patient demonstrated remarkable commitment to his treatment plan. Over the course of several appointments, I witnessed a profound cognitive and emotional shift in his attitude, as he eagerly worked to regain his smile. On my last day of rotation, I saw the patient’s joy upon viewing his new smile, thanks to the successful fitting of a removable partial denture. This experience underscored the importance of patience, empathy, and consistency in working with patients who have faced significant life challenges.
Another inspiring figure I encountered during my community rotations was Inga, a Dental Health Aide Therapist (DHAT) for Tulalip. She was deeply committed to keeping children out of general anesthesia by providing dental care in a traditional dental setting. I found it difficult to watch children undergo sedation for treatment due to their high caries risk and need for extensive restorative work. However, Inga’s approach, which focused on behavioral management and more frequent recalls, was particularly inspiring. I observed that children who received this approach were more likely to return for regular check-ups and even looked forward to their “happy visits.” This reinforced my own interest in applying behavioral management techniques and motivational interviewing to prevent the need for sedation and provide care in a less invasive, more positive setting utilizing minimally invasive dental practices.
These various encounters have had a lasting impact on my personal and professional development. They have deepened my understanding of the disparities in access to dental care and the importance of creative solutions to bridge these gaps. From mobile dental units to community-based financial assistance programs and more frequent recall visits, these experiences have reinforced the need for collaboration and a minimally invasive approach to patient care. As I continue to develop as a dental professional, I am committed to advocating for underserved populations and using the knowledge and skills I have gained to improve access to care in my future practice within my tribal community back home in Michigan.
My time working in various dental settings has been an eye-opening and rewarding experience. Through my work with high-risk communities, I have come to appreciate the role of communication, collaboration, and innovative care models in addressing their needs. These experiences have shaped my understanding of the dental profession and reinforced my commitment to promoting equitable access to dental care. Moving forward, I am eager to continue working with underserved communities, advocating for solutions such as dental therapy to aid in improving access to care and ensure that all patients can achieve optimal oral health.
My experiences showcase the need for additional resources to support community-based care such as a mobile dental units for Veterans and families unable to access traditional dental treatment models Mobile dentistry is in my future, and I am eager to be involved in the benefits and impact it can have on communities.